Regardless of all of the trending know-how adopted by insurance coverage leaders to draw new clients, the claims course of remains to be one of the vital essential experiences a present policyholder has with an insurance coverage supplier. And this conventional methodology of claims processing is difficult because of the massive quantity of labor within the hand of insurance coverage suppliers like sifting by means of paperwork to examine errors, assess dangers, and be sure that claims fee is initiated on time, which must be accomplished manually on time.
That’s how the claims processing typically turns into a “tail wagging the canine” state of affairs as acquiring correct and well timed paperwork and data requires a substantial quantity of group effort and time. This will trigger vital dissatisfaction amongst policyholders, who can simply take their enterprise elsewhere.
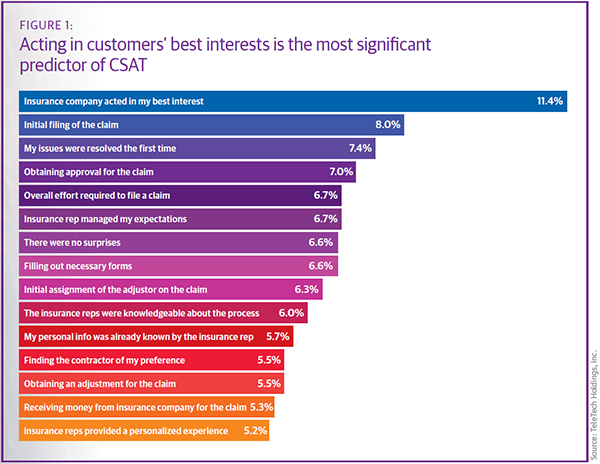
And everyone knows {that a} constructive buyer expertise is all insurance coverage leaders want to draw extra clients and speed up their ROI. In keeping with a report, the common buyer satisfaction stage extremely is dependent upon the effectivity of the preliminary claims processing. The under picture actually depicts the preliminary filling of claims and the competence of insurance coverage brokers.
So, how can insurance coverage leaders speed up claims processing and speed up the client satisfaction rating? Is there any answer? Let’s discover out the reply on this weblog.
Challenges in Handbook Claims Processing
Authorities rules and penalties, coupled with a consistently rising quantity of claims, exacerbate the established order that many insurers face – like slower decision occasions that frustrate clients and hovering operational prices attributable to error-prone information dealing with. Let’s have a look at the challenges confronted by insurers in brief-
-
Heavy Operational Price
Retaining prices in examine is all the time on the prime of the record whereas modernizing conventional claims processing. When techniques all throughout the group are usually not built-in, the claims agent should have to look throughout a number of techniques and sources to search out the precise data moderately than apply his decision-making to settle the claims. Additionally, insurer brokers additionally need to re-key the data between system or emails, CRM, and backend functions. This method introduces errors, frustration, and extra prices.
A recent study found that only 5% of insurers are fully digitized or automated. -
Lack of Constant Supply
It’s common for handbook claims processing to lack consistency and effectivity in process administration. A buyer could also be dissatisfied when an insurance coverage agent calculates totally different payouts for equivalent claims. Moreover, if one declare is given precedence over one other with out correct time administration, delays and inaccuracies can happen.
-
Poor Knowledge Integration
In claims processing, information integration is the technical course of of mixing information derived from a number of sources and making a centralized system. Moreover, the primary concern with information is coping with inaccurate and outdated information. A single error within the system results in buyer dissatisfaction and errors in initiating the claims fee that additional results in a dissatisfied buyer expertise.
According to a recent survey, only 30% of policyholders reported a positive experience with their insurance providers. -
Rising Claims Fraud
As per the report, insurance coverage claims fraud estimates loss is $308.6 billion within the 12 months 2022. Such malicious claims add as much as further pressure on insurance coverage brokers as lots of time have to be devoted to analyzing the authenticity of claims. And if analyzed manually it takes a very long time to examine the authenticity and probabilities of errors as effectively. That is one more reason that nearly 78% of shoppers are involved about insurance coverage fraud.
-
Rising Buyer Expectations
In terms of clients, comfort, and communication are on the prime of the record. Additionally with rising on-line claims administration insurers’ brokers are anticipated to be out there 24/7 to reply buyer queries. And with extra revolutionary gamers coming into the market coverage pricing and high quality is just not the one sufficient to retain clients.
How Automated Insurance coverage Claims Processing Work?
Claims processing includes a collection of steps earlier than claims fee is transferred to the purchasers. Utilizing automation applied sciences like RPA in insurance coverage claims processing lots of duties are concerned within the claims course of. Let’s see how automated claims processing work.
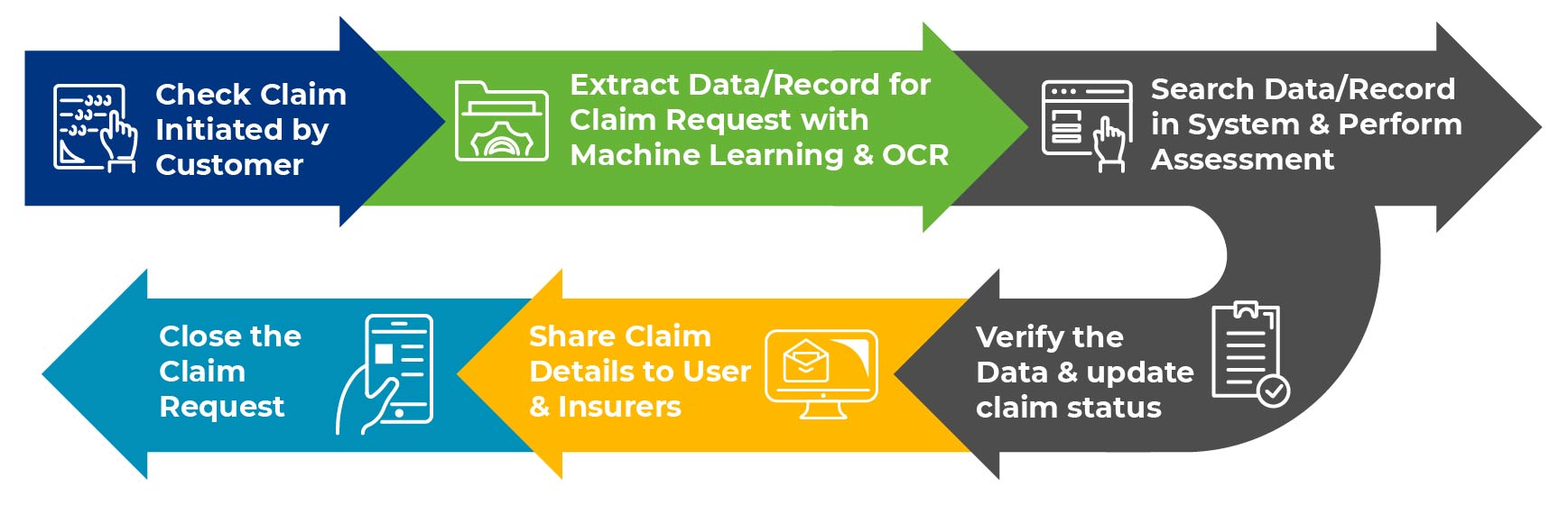
-
Knowledge Entry
To provoke the claims course of, insurers’ brokers needed to undergo lots of paper trails, emails and pdfs to extract information to examine the claims data. Reporting and processing this complete information right into a claims administration system, requires lots of focus and a focus. On this course of, utilizing clever RPA bots can automate the info entry process and scale back the probabilities of errors and velocity up the claims processing.
-
Claims Verification
As quickly as the info is entered into the claims administration system, insurers’ brokers need to undergo an intensive evaluation of claims paperwork initiated by customers. Insurers additionally need to be sure that each information that’s collected are correct, matches the regulatory compliance, and isn’t duplicated. RPA in insurance coverage claims processing can cross-verify and examine the claims information towards related database and guidelines and determines the quantity of compensation that’s payable. Going automation manner, insurance coverage brokers can probably detect fraud and scale back the time required to course of claims
-
Claims Adjudication
After claims verification, RPA will help insurance coverage brokers in figuring out the eligibility of claims by evaluating them towards the pre-determined guidelines set by insurers. AI-enabled RPA in insurance coverage claims processing can simply flag claims that require consideration and be sure that claims are adjudicated precisely and effectively. Additionally, an RPA chatbot will help in interesting for claims in case claims are denied.
-
Claims Settlement and Communication
As quickly as claims information is verified and settlement is completed, insurance coverage brokers want to speak with policyholders for sending out notifications and reminders. Right here as an alternative of people sharing data, RPA bots may be leveraged to share data. This guidelines out the requirement of providing operational availability 24/7 for claims processing and reduces the workload for people.
Advantages of Automated Claims Processing
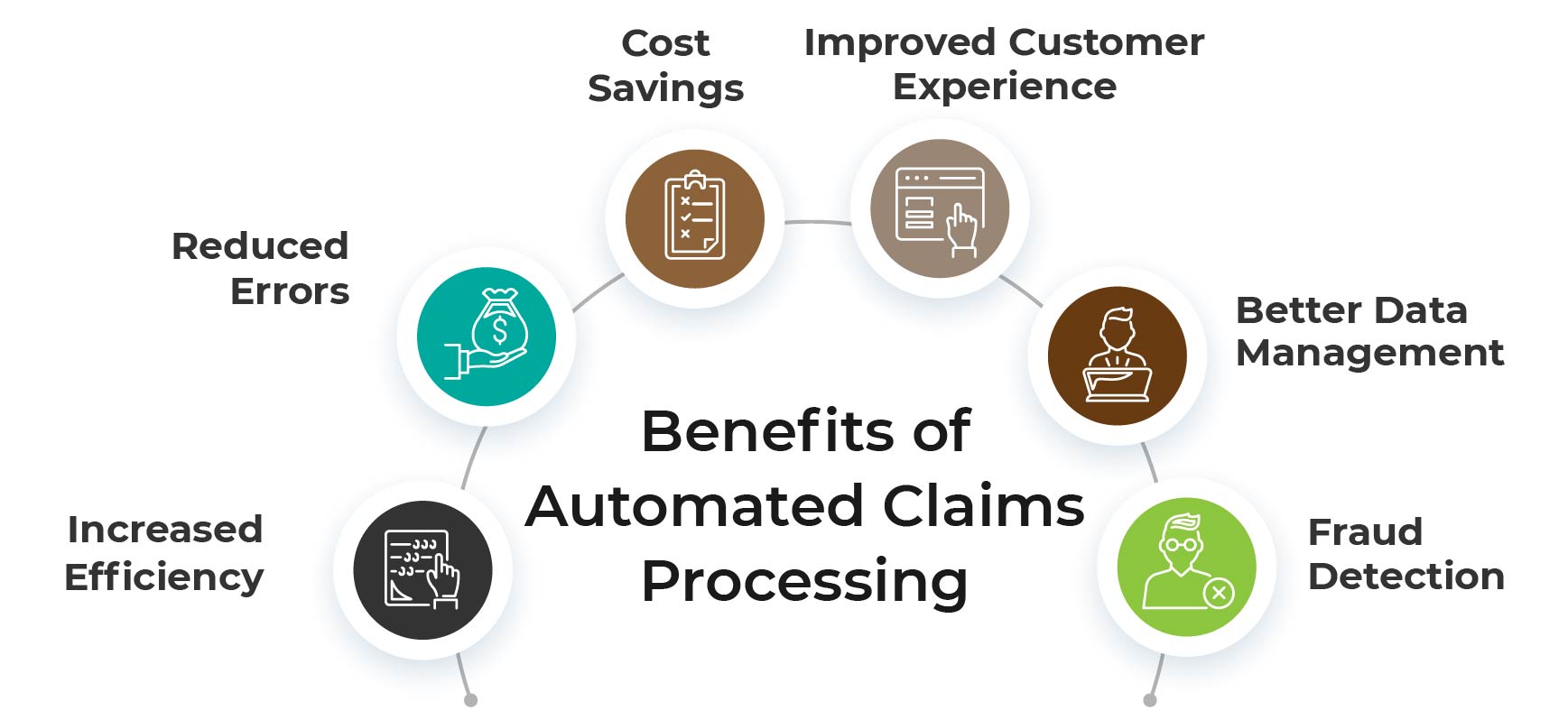
Automated claims processing can convey a number of advantages to insurance coverage firms, together with
-
Elevated Effectivity
Automated claims processing can scale back the effort and time required to course of claims. Because of this claims processing is completed extra shortly, and sources may be allotted extra effectively.
-
Lowered Errors
Utilizing clever RPA bots can decrease the chance of errors and omissions. This will help to make sure that claims are processed precisely and that claimants obtain the suitable compensation.
-
Price Financial savings
Having RPA bots care for the info reporting and verification duties can scale back the price of claims processing. As value is diminished, insurance coverage brokers can higher use the cash for implementing RPA options in different insurance coverage processes.
-
Improved Buyer Expertise
Automated claims processing can enhance the client expertise by decreasing processing occasions and offering sooner and extra correct claims choices. This will help to extend buyer satisfaction scores and ensure these clients keep longer together with your group.
-
Higher Knowledge Administration
Utilizing clever doc processing bots will help to enhance information administration by capturing and storing information in a extra structured and arranged method. This will make it simpler to research information and establish patterns that can be utilized to enhance claims processing.
-
Fraud Detection
Automated claims processing may also assist to detect fraudulent claims by utilizing machine studying and synthetic intelligence to establish anomalies and inconsistencies in claims information.
Conclusion
As buyer wants change quickly and competitors will increase, insurers proceed to face challenges. Moreover, insurers have begun implementing RPA in back-office processes to automate transactional, routine, rule-based duties throughout which capital and expertise are repurposed to handle extra complicated and strategic challenges. Utilizing robotic course of automation in insurance coverage can promote long-term success and productive market alternatives. Resulting from its versatility and benefits, automation will undoubtedly be adopted within the insurance coverage sector as effectively.